ABSTRACT
Background
The rarity of severe diseases following COVID-19 infection balanced against rare COVID-19 vaccination-related adverse effects is an important consideration for vaccination policies. We aimed to assess the short-term and long-term risks of vascular and inflammatory diseases following first COVID-19 diagnosis and vaccination in children and young people.
Methods
In this retrospective, population-based cohort study, we analysed whole-population linked electronic health records for all individuals in England aged younger than 18 years, registered with a general practitioner, and with known age, sex, and region of residence, between Jan 1, 2020, and Dec 31, 2022. Outcomes were arterial thrombotic events, venous thrombotic events, thrombocytopenia, myocarditis or pericarditis, and inflammatory conditions. COVID-19 diagnosis was defined as the earliest record of a positive SARS-CoV-2 PCR or antigen test, or a COVID-19 diagnosis code in primary-care or secondary-care records; COVID-19 vaccination was defined as the earliest documented receipt of the BNT162b2 vaccine (the predominant vaccine during the study period). Adjusted hazard ratios (aHRs) for all outcomes were estimated by time since a first COVID-19 diagnosis during Jan 1, 2020–March 31, 2022 and by time since a first COVID-19 vaccination during Aug 6, 2021–Dec 31, 2022, adjusting for age, sex, ethnicity, region, deprivation, general practitioner contact frequency, and medication use.
Findings
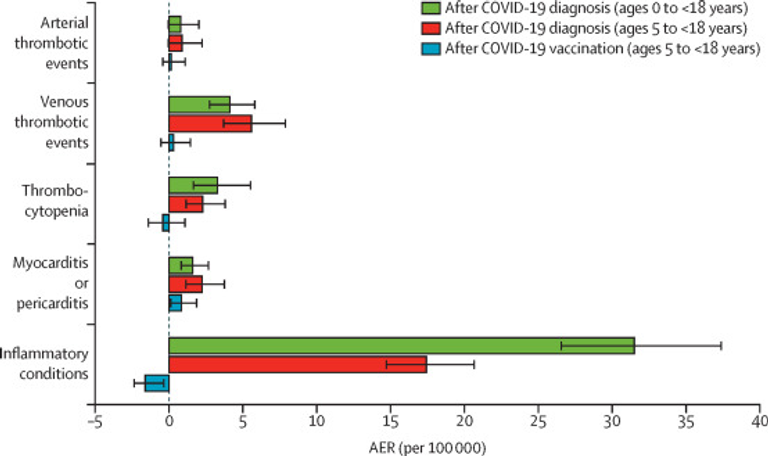
Of 13 896 125 individuals younger than 18 years (6 784 260 [48·8%] female and 7 111 865 [51·2%] male; 9 979 420 [71·7%] White), 3 903 410 (28·1%) had a COVID-19 diagnosis. COVID-19 diagnosis (compared with no or before diagnosis) was associated with higher risk of arterial thromboembolism (aHR 2·33 [95% CI 1·20–4·51]), venous thromboembolism (4·90 [3·66–6·55]), thrombocytopenia (3·64 [2·21–6·00]), myocarditis or pericarditis (3·46 [2·06–5·80]), and inflammatory conditions (14·84 [11·01–19·99]) in the first week after diagnosis. Incidence declined in weeks 2–4, but remained elevated to beyond 12 months for venous thromboembolism (1·39 [1·14 –1·69]), thrombocytopenia (1·42 [1·01–2·00]), and myocarditis or pericarditis (1·42 [1·05–1·91]). Among 9 245 395 individuals aged between 5 and younger than 18 years who were eligible for vaccination (4 510 490 [48·8%] female and 4 734 905 [51·2%] male; 6 684 140 [72·3%] White), 3 407 560 (36·9%) received a first vaccine. COVID-19 vaccination (compared with no or before vaccination) was associated with elevated risk of myocarditis or pericarditis within the first 4 weeks after vaccination (1·84 [1·25–2·72]). The 6-month absolute excess risks for myocarditis or pericarditis were 2·24 (1·11–3·80) per 100 000 individuals after diagnosis versus before diagnosis or undiagnosed, and 0·85 (0·07–1·91) after vaccination versus before vaccination or unvaccinated.
Interpretation
Children and young people have higher risks of rare vascular and inflammatory diseases up to 12 months after a first COVID-19 diagnosis and higher risk of rare myocarditis or pericarditis up to 4 weeks after a first BNT162b2 vaccine, although the risk following vaccination is substantially lower than the risk following infection. These findings are of great importance for national policy makers and caregivers considering vaccination consent for children, and support the public health strategy of COVID-19 vaccination in children and young people to mitigate the more frequent and persistent risks associated with SARS-CoV-2 infection.
Funding
Wellcome Trust, British Heart Foundation Data Science Centre, and Health Data Research UK.