ABSTRACT
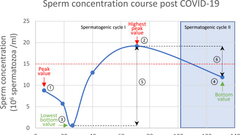
The COVID-19 pandemic has yielded substantial evidence indicating that SARS-CoV-2 may impair reproductive function, particularly by adversely affecting sperm quality. Given the potential implications for male reproductive health, it is crucial to assess the reversibility of such damage, determine the precise recovery timeline, and evaluate post-infection health parameters. Male patients who had undergone sperm analysis prior to SARS-CoV-2 infection were enrolled to evaluate longitudinal changes in sperm quality during a 6-month recovery period. Sperm parameters were collected at five consecutive time points: before infection and at 1, 2, 3, 6 months post-infection. Additionally, quality of life (QoL), psychological status, and sexual function were evaluated via standardized questionnaires within the first month after infection. The primary outcomes were sperm concentration and progressive motility. Generalized Estimating Equations (GEE) were applied for statistical analysis of repeated measures, while Kaplan–Meier survival analysis was used to assess temporal trends in sperm recovery. 1009 subjects underwent sperm analysis during widespread COVID-19 transmission, from April 2022 to January 2023. Among them, 139 eligible patients completed sperm analysis in the first month post-infection, with 92 (66%) patients were tested in the second month, 72 (52%) patients in the third month, and 64 (46%) patients completed the sperm analysis in the sixth month. The final analytical cohort comprised 74 participants with complete pre-infection baselines and ≥ 3 post-COVID-19 semen analyses at specified intervals (1, 2, 3, 6 months). Sperm concentration [39.22 (95% CI 32.02–46.41)] and progressive motility [36.41 (95% CI 32.29–40.53)] showed a significant decline at 1-month post-infection compared to pre-infection levels. Partial recovery occurred during the second and third months, though values remained significantly lower than baseline pre-infection levels at 6-month follow-up (p < 0.05). Kaplan–Meier analysis estimated median recovery times of 5 months (95% CI 4.57–5.43) for sperm concentration and 3 months (95% CI 2.08–3.82) for progressive motility, with no age-dependent differences observed (log-rank p > 0.05). Comprehensive assessments showed preserved psychological status, quality of life, and urogenital function at 1-month post-infection. Sperm quality was negatively impacted by COVID-19 infection, but temporary, with a recovery period of 3–5 months. Furthermore, no abnormalities were observed in men’s psychological, urinary symptoms, or sexual function during the initial month following recovery from infection.